Overview
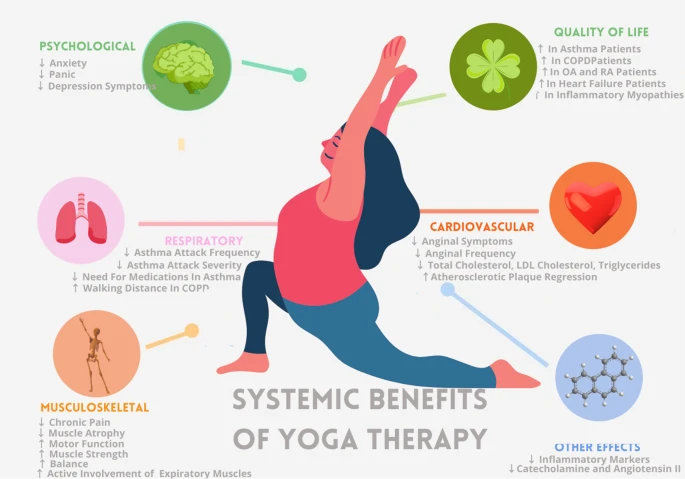
Therapeutic yoga is an evidence-based approach that supports Chronic disease management alongside medical treatment. Unlike general yoga, it is personalized, medically guided, and adapted to individual conditions. Research shows benefits across hypertension, diabetes, arthritis, and cardiovascular disease by reducing stress, inflammation, and improving physical function.
Managing Chronic Conditions Through Yoga: Evidence-Based Approaches for Patients
Systemic benefits of yoga therapy across psychological, respiratory, cardiovascular, musculoskeletal, and inflammatory health pathways.
Beyond Medication Alone
In the case when Rita was told to include a third blood pressure medication, she questioned what she could do. Her doctor recommended therapeutic yoga to be added to her current treatment. Her blood pressure stabilized and her quality of life got better six months later.
Medication is often used in chronic disease management. Although necessary, drugs may not necessarily treat stress, inflammation, or deterioration. There is a growing demand among patients to find safe and evidence-based and clinically suitable complementary strategies.
One of such methods has been yoga. When used as a part of therapy and under appropriate guidance, it may complement the usual care and generate better results in patients.
Understanding Therapeutic Yoga
Why General Yoga Is Not Enough
The majority of community-based yoga classes are catered to healthy individuals. They are centered on fitness, flexibility and group instruction as opposed to medical requirements. This method can be unproductive or dangerous in the case of chronic patients.
Yoga as therapy is an exception. It is personalized, adapted and oriented by clinical evidence. Practices are modified according to medical goals, health history and functional limitations.
What Makes Yoga Therapeutic
Therapeutic yoga begins with analysis. Medical history, medications, and symptoms are reviewed by instructors prior to the development of a program. Movements, breathing and relaxation are chosen deliberately.
The sessions focus on safety, slow progress, and collaboration with the medical professionals. Yoga is appropriate to use with patients who deal with complicated conditions.
Understanding the distinction between general yoga and therapeutic applications is essential for both patients and practitioners. Programs that specialize in therapeutic yoga provide the depth of training necessary to work safely with clinical populations. Those interested in exploring how yoga can be tailored to medical conditions can learn about the program that integrates evidence-based practices with individualized assessment protocols.
Yoga for Hypertension
Clinical Evidence
Various clinical studies indicate that yoga is able to reduce blood pressure. The meta-analyses state that systolic blood pressure and diastolic blood pressure reductions of about 11 points and 6 points in adults with hypertension.
These improvements are most pronounced when yoga is practiced regularly. Results are comparable to first-line lifestyle interventions when used alongside medication.
Gentle yoga postures support blood pressure regulation by improving vascular function and calming stress driven nervous system activity.
Physiological Mechanisms
Yoga lowers the sympathetic nervous system activity. This reduces the heart rate, reduces vascular resistance, and enhances endothelial activity.
Relaxation and slow breathing also inhibit cortisol and adrenaline. These modifications facilitate blood pressure regulation.
Safety Considerations
The patients are advised to take all the prescribed medications. Regular blood pressure monitoring needs to be noted particularly at the start of practice.
Inversions, breathing, and extreme poses are not taken. Professionals who are conversant with cardiovascular conditions should guide yoga.
Yoga for Type 2 Diabetes
Clinical Evidence
There are over eighty clinical studies that show the usefulness of yoga in type 2 diabetes. Research indicates a decrease of between 0.5 to 1.0 percent in HbA1c.
Yoga also enhances the level of insulin sensitivity and abdominal fat loss. Such modifications assist in glucose control in the long run.
Physiological Mechanisms
Yoga increases glucose uptake in the muscles and efficiency. Reduction of stress decreases the cortisol which in turn increases blood sugar levels.
Exercise also helps in the normal functioning of the pancreas and lowers the inflammation associated with diabetic complications.
Safety Considerations
Before and after sessions, patients are to monitor their blood glucose. Depending on the prescriptions, medication time can be changed under the supervision of physicians.
Yoga is not taken in hypoglycemic episodes. Referral to an endocrinologist is advisable.
Yoga for Arthritis
Clinical Evidence
The quality of evidence that systematic reviews offer on pain reduction and functional improvement in patients with arthritis is moderate. It has been shown to be beneficial in osteoarthritis as well as rheumatoid arthritis, especially when yoga is done regularly for a few weeks.
Longitudinal studies indicate a long-term increase in the degree of pain, grip strength, and joint mobility. The participants also indicate that they have gained confidence in movement and have less dependency on pain medication.
Physiological Mechanisms
Yoga enhances the range of motion in joints without loading on the joints. Tone strengthening of the muscles around the joints lessens the stress load of the joints, better alignment and increases the overall stability of the joints.
CRP and IL-6 are inflammatory factors, which are reduced during regular practice. Balance and proprioception are other areas that can be improved to reduce the risk of falls and maintain functional independence.
Safety Considerations
Yoga is not to be used when the inflammatory exacerbation is acute. The movement is slow, assisted, and never by the use of pain or limited movements.
Chairs, blocks, and straps are some of the props that relieve stress on the joints and make them more accessible. Safety requires that the people teaching arthritis populations should be those with experience.
Yoga for Cardiovascular Disease
Clinical Evidence
Studies have indicated that yoga leads to improvement in cardiovascular risk factors, which is as good as traditional low to moderate exercise. There is an increased exercise tolerance, decreased anxiety, and general quality of life.
Research also proves the improvement of cholesterol patterns and heart rate variability. The changes lead to cardiovascular resilience in the long term.
Physiological Mechanisms
Autonomic control of the lower heart rate and blood pressure is achieved through yoga. Improved vagal tone facilitates effective cardiac performance and recovery to stress.
Diluted sympathetic decreases inflammation and platelet aggregation. These are the complementary effects of structured cardiac rehabilitation programs.
Safety Considerations
Before starting to practice yoga, it is necessary to get the clearance of the physicians. Sessions are soft, gradual and do not involve breath retention and effort.
Professional training in cardiac populations should be used in teaching. Constant interaction with the medical team is advisable.
How Yoga Works Across Conditions
Nervous System Regulation
Yoga restores the body to a state of recovery instead of being in a state of chronic stress. Parasympathetic stimulation enhances the digestion, quality of sleep and the immune system.
There is an increase in heart rate variability which means that the body is more resilient to physical and emotional stress. This mechanism benefits a wide range of chronic conditions.
Inflammation Reduction
There are numerous chronic diseases with which inflammatory pathways are common. Combined movement, regulation of breath, and stress reduction of yoga inhibit pro-inflammatory cytokines.
These alterations can be determined in blood factors. Reducing inflammation helps in maintaining symptoms and retarding the disease.
Stress Hormone Balance
Yoga reduces cortisol and adrenaline in the long term. Less hormonal burden enhances metabolism and tissue remodelling.
Excessive management of chronic stress improves disease management. Patients usually complain of better energy, mood and everyday functioning.
Safety and Contraindications
General Guidelines
Before starting, the patients are supposed to seek physician clearance. Instructors should be informed about all conditions and drugs.
The practice starts slowly and gradually. Medical review should be done on any worrying symptoms.
Condition-Specific Cautions
Cardiovascular patients avoid inversions and strain. Hypertensive patients avoid breath retention and head-down positions.
Diabetic patients are careful about their glucose. The range of motion is painful to avoid in arthritis patients.
Finding Qualified Practitioners
Credentials That Matter
The teachers must possess a minimum of 200-hour certification in yoga. It is highly encouraged to have further training in therapeutic or medical yoga.
It requires experience in the medical population. The anatomical, pathological and contraindication knowledge enhances safety.
Professional Training Standards
High-level training equips practitioners to deal with chronic conditions in a safe manner. Such programs include assessment, modification and clinical protocols.
Integrating Yoga With Medical Care
A Team-Based Approach
Yoga does not substitute medical treatment; it is complementary to it. Inter-provider communication facilitates coordinated care.
Patients are expected to share the information about yoga practice with their healthcare team. Development and progress and symptoms need to be openly shared.
Empowered, Evidence-Based Care
Moving Forward Safely
Having a chronic illness means constant care. Therapeutic yoga offers the means that patients can employ on a daily basis.
Yoga, when done in safe and evidence-based practice, improves the quality of life. It gives the patients the power to be active in their health process.
Conclusion
When practiced safely under professional guidance, therapeutic yoga complements medical care by enhancing quality of life and long-term health. It empowers patients to actively participate in managing chronic conditions with confidence and safety.