Can endometriosis occur after a hysterectomy?
Yes, it is possible to experience endometriosis after a hysterectomy.
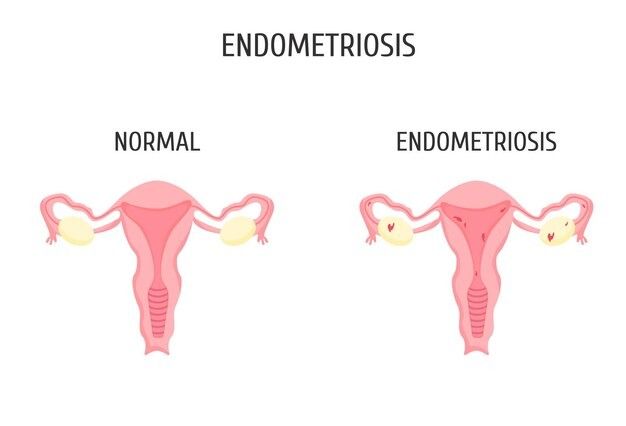
Endometriosis is a common gynecological condition affecting millions of women worldwide. In some cases, a hysterectomy is recommended as a definitive treatment option when no other treatment works. Once a hysterectomy is done the pain gets better. However, surprisingly, some women experience endometriosis symptoms even after undergoing this procedure. It might come back, especially in the bowels. If bowel hysterectomy after endometriosis symptoms are visible, then it was probably there before. Endometriosis is not caused by hysterectomy.
In this article, we will explore the reasons for "Endometriosis after hysterectomy" and dig deeper into the potential reasons behind this perplexing issue.
Your health is too important to ignore – schedule your appointment now.
Why can there be a persistence of endometriosis after hysterectomy?

Even after hysterectomy or menopause, endometriosis can still persist. While some people feel better after these. Endometriosis after hysterectomy can still persist. It sticks around with other similar conditions like adenomyosis or fibroids. These can also cause pain. Removing the uterus might help with some symptoms. But endometriosis following hysterectomy can keep causing trouble. Also, endometriosis can make estrogen on its own for its growth. Hence, it does not need ovaries to produce estrogen for it.
So, yes endometriosis after hysterectomy is possible. Let's check the reason for persistence.
The persistence of endometriosis after a hysterectomy can occur for several reasons:
- Remaining Endometrial Tissue: Sometimes, small pieces of endometrial tissue can be unintentionally left behind during a hysterectomy. These fragments may grow and result in symptoms of endometriosis.
- Extra-Uterine Endometriosis: Sometimes, endometrial tissue can attach itself to places outside the uterus, like the ovaries, fallopian tubes, or pelvic cavity. If these implants are not removed during a hysterectomy, they can persist and lead to symptoms of endometriosis.
- Hormonal Influence: Although a hysterectomy removes the uterus, it does not guarantee the complete elimination of all hormonal influences in the body. The presence of hormonal imbalances, specifically changes in estrogen levels, has the potential to trigger any remaining endometrial tissue or implants, thus leading to the persistent occurrence of endometriosis.
- Incomplete Surgery: In some cases, the surgical removal of endometrial tissue during the hysterectomy may not be thorough enough. If the surgeon fails to remove all endometrial lesions or implants, the condition can continue to develop.
- Misdiagnosis: Sometimes, the symptoms that persist after a hysterectomy may not actually be due to endometriosis but may be caused by other medical conditions with similar symptoms. This misdiagnosis can lead to the belief that endometriosis has persisted.
- Reactive Changes: In response to the surgery itself, the body may undergo reactive changes that can mimic endometriosis symptoms. Imaging tests and laparoscopy may be required to confirm the presence of endometriosis after a hysterectomy.
It's essential to consult with your doctor if you suspect the persistence of endometriosis after a hysterectomy. Accurate diagnosis and appropriate treatment options can help manage and alleviate the symptoms effectively.
Read carefully!! This will help you in Recognizing Persistent Endometriosis Symptoms.
Take charge of your health and your life. Contact us today!
What are the symptoms of persistent endometriosis after a hysterectomy?

symptoms of persistent endometriosis after a hysterectomy
The signs of endometriosis can change based on where and how much of that tissue is there. Some common signs are:
- Terrible period pain.
- Bleeding between periods when you're not supposed to.
- Hurting during sex.
- Pain when you pee.
- Bleeding or hurting when you go to the bathroom.
- Always have pelvic pain.
- Feeling all swollen.
- Feeling sick and throwing up.
- Feeling exhausted.
Let's explore what are the treatment for endometriosis after hysterectomy!!
Take charge of your health and your life. Contact us today!
What treatment options are available for persistent endometriosis after a hysterectomy?

There's no cure for endometriosis, but there are treatments to help with the symptoms. The main treatments for endometriosis after hysterectomy are:
- Hormone Therapy: Some medicines can slow down the growth of endometrial tissue. They block certain hormones. These include birth control pills, progestin, and GnRH medications.
- Pain Relief: Managing pain is essential. You can use over-the-counter drugs like NSAIDs. If they don't work, your doctor might prescribe stronger pain medicine.
- Surgery: If your pain is severe and other treatments don't help, your doctor might suggest surgery. They can remove the problematic tissue through a procedure called laparoscopy.
Preventing Recurrence: Is It Possible?
Is it possible to prevent the recurrence of endometriosis after hysterectomy?

Symptoms of endometriosis can resurface after a hysterectomy, leading to the resurgence of pelvic pain. The outcome of the surgery is determined by how effectively it removes all the problematic tissue. The only way that may reduce the risk of endometriosis is surgery. The goal of the surgery is to completely get rid of these tissue spots. This minimizes the chances of endometriosis after hysterectomy.
Managing Symptoms Through Lifestyle Changes! Understand what you can do.
Can lifestyle changes help manage persistent endometriosis symptoms?

- Exercise: Engaging in activities like running or biking can lower estrogen levels. This reduces endometriosis after hysterectomy symptoms and pain sensitivity.
- Diet: Adopt a plant-based diet with fruits, vegetables, and fish. Try limiting red meat and alcohol consumption.
- Heat Therapy: Applying a warm pad or taking a warm bath can help alleviate endometriosis after hysterectomy pain.
- Stress Management: Practice relaxation techniques like deep breathing and meditation. Seek counseling to reduce stress that can worsen symptoms.
- Massage: Gentle massages can soothe sore muscles and relieve endometriosis pain.
- Acupuncture: This traditional therapy can help reduce endometriosis pain by stimulating pressure points in the body.
- Emotional Support: Consider therapy, support groups, or confiding in friends and family to manage the emotional impact of endometriosis.
Can endometriosis be cured permanently?
Endometriosis is a chronic medical condition for which there is no permanent cure. However, there are several medical and surgical treatments available to manage the symptoms and improve a person's quality of life.
Your well-being is our priority - call us to book your appointment today.