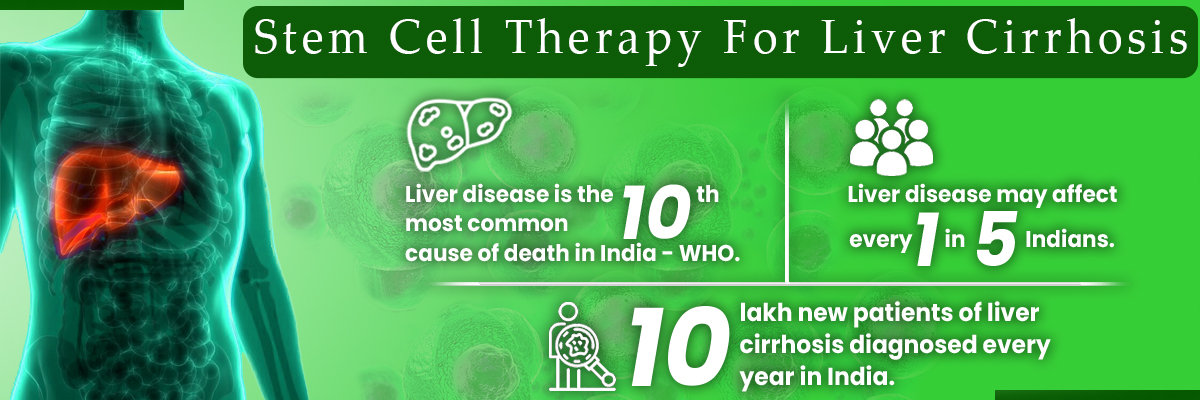
Introduction
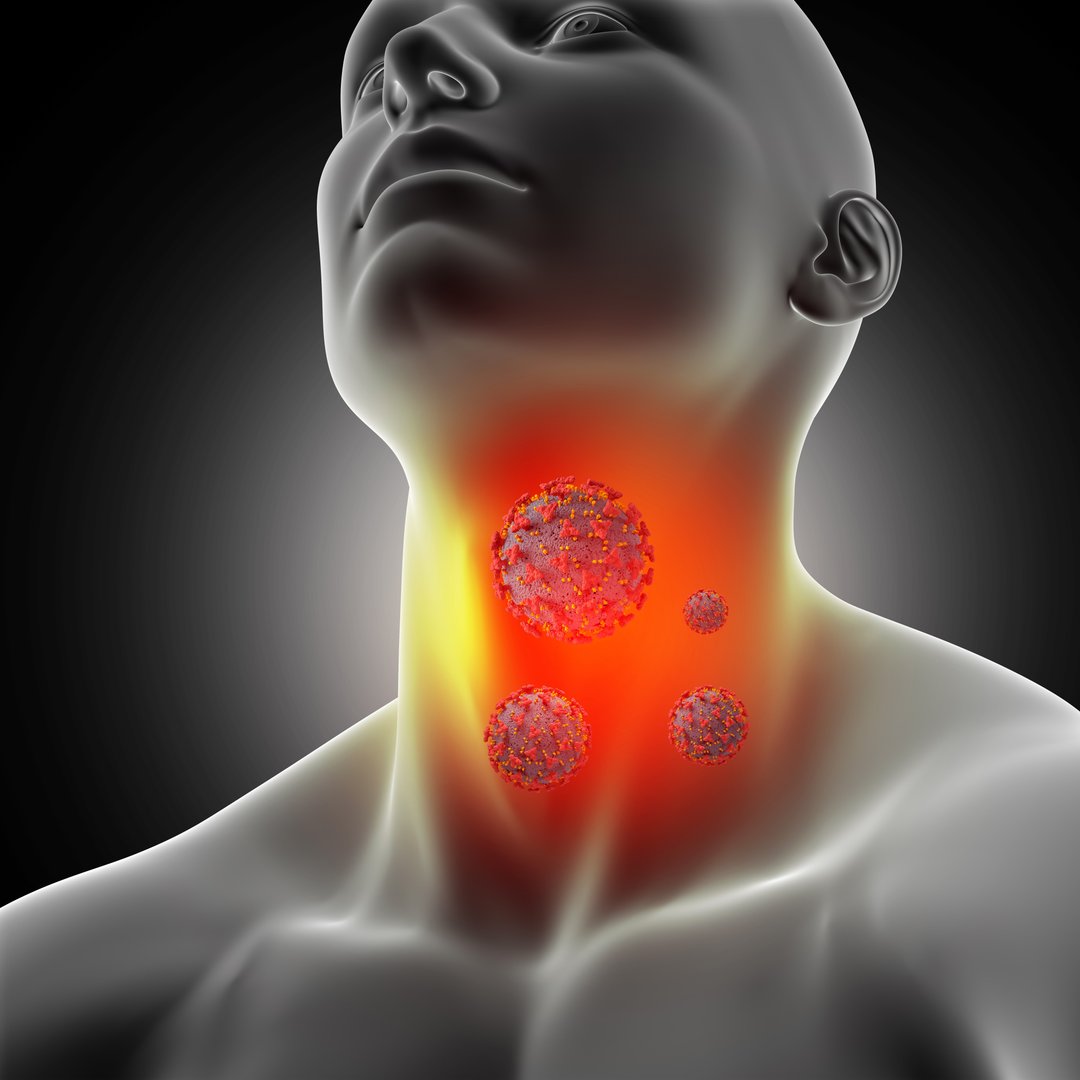
Hashimoto's disease is an autoimmune condition in which the immune system mistakenly attacks the thyroid gland, resulting in chronic inflammation and the thyroid gland's inability to function properly. Although traditional treatments include thyroid hormone medication replacement and periodic monitoring, emerging medical technologies such as stem cell therapy are being promoted. Stem cell studies today are opening up opportunities for increasingly targeted treatments that extend far beyond symptoms. While still not very mainstream, this treatment may be a revolution shortly in how we're treating not only Hashimoto's but other thyroid diseases — even thyroid cancer.
What Is Hashimoto's Disease
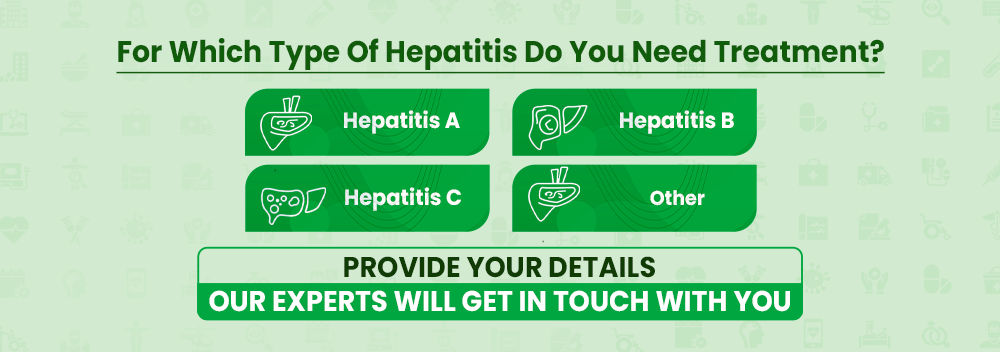
Hashimoto's thyroiditis is the leading reason for hypothyroidism, especially in women. The disease slowly destroys the thyroid gland and impairs the production of necessary thyroid gland hormones. The majority of patients receive thyroid tests to track TSH levels and begin lifelong hormone replacement therapy.
In certain situations, uncontrolled chronic thyroid inflammation has also been found to raise risks of thyroid cancer development. With everything that has been developed in the treatment of thyroid cancer, even so, there is no light at the end of the tunnel as far as stopping thyroid diseases altogether. That is where therapies such as regenerative stem cells come into play. Connect with specialists to receive professional advice on stem cell treatment and its application in Hashimoto's disease.
How Stem Cells Can Assis In Hashimoto's Disease
Stem cell therapy targets the body's internal repair systems. In autoimmune thyroid conditions such as Hashimoto's, the immune system strikes against the thyroid gland by mistake. Stem cells — especially mesenchymal stem cells — possess immunomodulatory capability that can in all likelihood quell such untargeted immune system attacks. Such cells potentially can dampen inflammation, trigger the regeneration of thyroid tissue, and enhance hormonal function over a period of time. If you want more in-depth information about stem cell treatment you can book a doctor's video consultation on our platform in minutes.
Types Of Stem Cells Used In Treatment
Cell Types Used Stem cell therapy is not an off-the-shelf product. Several types of stem cells are under investigation for their specific potential to modulate the immune system and repair tissue. Before the exploration of treatment, keeping in mind the central cell types involved in the therapy is essential. Types of stem cells used:
- Mesenchymal Stem Cells (MSCs): MSCs are the most studied and utilized to treat autoimmune diseases. Derived from bone marrow, fat tissue, or umbilical cord, MSCs modulate the immune response and secrete anti-inflammatory cytokines. Increasingly applied to thyroid-related autoimmune diseases like Hashimoto's because MSCs can restore thyroid gland function.
- Embryonic Stem Cells (ESCs) & Induced Pluripotent Stem Cells (iPSCs): They are pluripotent stem cells capable of differentiating into any type of cell, including thyroid cells. While they have great promise in regrowing lost or damaged thyroid tissue, they are more experimental and create ethical, regulatory, and safety issues.
Evidence From Research & Studies
Increasing demand for therapy and storage of stem cells has motivated many studies assessing its impact on autoimmune thyroid disease. It is also seen that the success rate of treatment is much higher when consulted by the best stem cell doctors in India. Below are some of the evidences:
Benefits Of Treatment
Stem cell therapy has the potential to cure autoimmune thyroid diseases. Patients can expect enhanced levels of energy, decreased inflammation, and more accurate control of thyroid hormones without being entirely reliant on thyroid medications. It may also retard the process of disease and decrease the likelihood of developing associated complications like thyroid cancer. The value-added aspect is that this treatment may address the root cause of immune compromise — something conventional therapies do not provide.
Risks Associated With The Treatment
As great as stem cell therapy sounds, there must be recognition of risk. These can be immune rejection, infection, creation of undesired cell types, and the unknown long-term of what these cells will have done in the body. There are also ethical issues of working with embryonic stem cells. Also, as the therapy is not FDA-approved, it's largely unregulated and has wildly varying safety and quality based on where it's being done.
Limitation Of The Treatment
Although stem cell therapy can potentially change the way thyroid disease is treated, it is under several limitations:
- Not FDA-approved for Hashimoto's: Stem cell therapy for Hashimoto's disease is still experimental. It is not FDA-approved or usually utilized in standard endocrinology practice.
- Cost & Accessibility Concerns: The cost of stem cell preservation and the cost of stem cell storage are considerations against most patients. As compared to traditional thyroid tests and treatments covered by insurance, stem cell procedures are generally out-of-pocket and, therefore less available to the average patient.
What Supportive Services May Be Continued With The Treatment
Even if a patient comes for stem cell therapy, it cannot be used as an independent cure. Adjunctive treatments are very important for control of symptoms and hormonal homeostasis:
- Hormone Replacement: The patients will still probably have to continue taking levothyroxine or other hormone medication for thyroid function during and after stem cell therapy.
- Lifestyle, Diet & Supplements: A positive lifestyle — thyroid-supportive diet, stress reduction, and certain supplements such as selenium — can improve results and decrease inflammation.
- Other New Therapies: The pairing of stem cell therapy with new immunotherapy medications or regenerative therapies may provide more improved, more individualized treatment protocols in the future.
Future Scope Of Treatment
The future for stem cell therapies for thyroid disease is bright. With further research, validating its safety and efficacy, we can predict more defined guidelines, reduced stem cell storage fees, and increased availability. With time and time gone by, stem cell banking will become an integral part of standard personalized medicine, not only for Hashimoto's, but thyroid cancer as well as other autoimmune conditions.
Summary
Although stem cell therapy is not yet the complete solution to thyroid disease eradication, it has immense potential. It targets the immune system and allows tissue repair, which attacks the fundamental cause of Hashimoto's that standard thyroid cancer treatment or hormone replacement cannot do as successfully. As stem cell technology advances, therapy is bound to move from experimental to accepted treatment, with real hope for millions.